
How to Reverse Insulin Resistance in PCOS
Nov 07, 2022Believe it or not, the majority of women I work with who have insulin resistance & PCOS, don't have these issues because of poor diet and eating too many carbs.
Sure, they may have grown up drinking soda, eating too many sweets and processed foods, however even after switching over to a 'healthy diet', many women continue to struggle with insulin resistance.
The solution isn't just cutting out carbs completely. There are other factors that need to be addressed in order to fully heal.
What IS Insulin Resistance?
It is believed that around 80% of women with Polycystic Ovarian Syndrome (PCOS) have some degree of insulin resistance. Insulin resistance occurs when our cells become 'numb' to the hormone insulin.
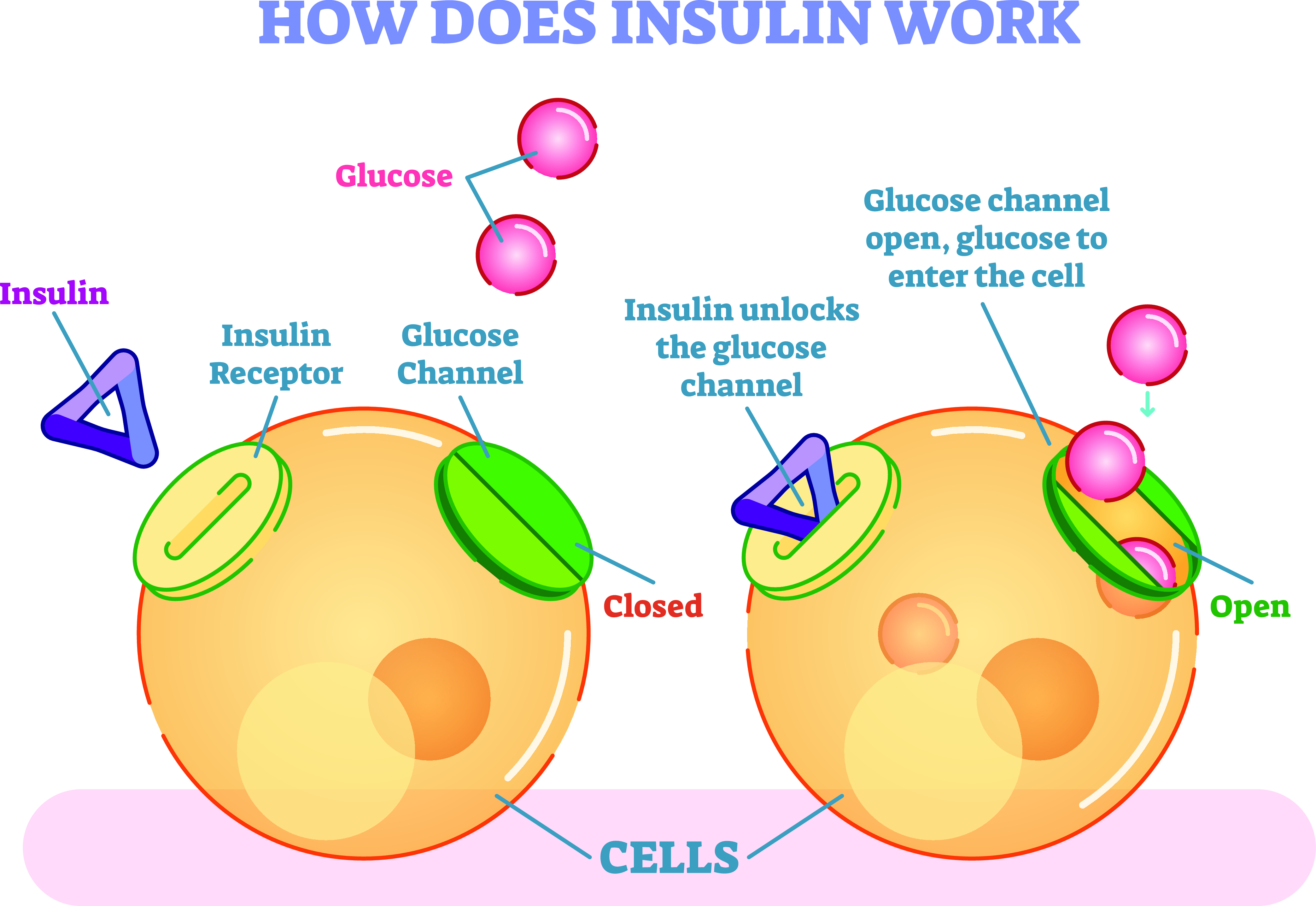
When we consume food (mainly carbohydrates), our blood glucose levels rise. This signals our pancreas to release the storage hormone insulin, which acts like a key, unlocking our cells and letting glucose in, to be used as fuel.
If the key or lock becomes damaged (aka our insulin hormone or cell receptors) then glucose remains elevated in the bloodstream and the cells are 'starving for energy'.
Our pancreas continues to pump out insulin as a way to try and lower blood glucose and fuel the cells, however in women with PCOS, insulin also stimulates the 'theca cells' in the ovaries to produce androgens like testosterone.
Androgens drive the common symptoms such as hirsutism (abnormal face/body hair growth), male pattern hair loss, cystic acne and can also halt ovulation, therefore affecting fertility and our menstrual cycles.
Long term, chronically elevated insulin and blood glucose levels increase our risk of type 2 diabetes, metabolic syndrome, obesity, cardiovascular disease, chronic inflammation and even certain types of cancer.
Some women may be VERY insulin resistant (bordering on type 2 diabetes) and unable to metabolise glucose effectively, whereas others have very mild insulin resistance, which may be causing hormonal imbalances, yet doesn't show clearly on conventional lab tests.
Common Indicators of Insulin Resistance....
- Weight gain
- Difficulty loosing weight
- Fat storage particularly around the midsection
- Skin tags
- Velvety patches of skin (Acanthosis Nigricans)
- Sugar/carb cravings
- Blood sugar instability
- A family history of Type 2 Diabetes
- Fatigue after eating (especially carb rich meals)
- Elevated liver enzymes or fatty liver disease
- Acne
- Frequent urination
- Excessive thirst
It is important to note that you can be at a 'normal' weight and still have insulin resistance. There are also different degrees of insulin resistance, even lean women can be struggling with this. If you are overweight or obese, it is likely that insulin resistance is playing a role in your PCOS.
Potential Downsides of Going TOO Low Carb...
Even though a low carb/ketogenic diet might temporarily lower blood glucose & insulin levels and maybe even improve things like weight loss or acne, insulin resistance tends to be a multifactorial condition, meaning that just changing one factor, usually isn't enough.
In fact, going too low carb, or for too long, may actually induce 'physiological insulin resistance'. Your brain requires glucose to function optimally, and when levels are low, peripheral insulin resistance is triggered. This causes your muscles to stop taking up this 'precious' glucose, so that your brain can be fuelled.
The 'great feeling' people can experience on a low carb diet is often due to the release of stress hormones, like cortisol, which actually breaks down your muscle tissue to raise blood glucose levels. Yes, you may lose weight, but you are actually sacrificing your lean muscle mass and potentially lowering your metabolic rate in the long term.
If you feel like you can't increase your carbohydrate intake after being on a low carb/keto diet, without gaining weight, breaking out or feeling like you're on a blood sugar rollercoaster, this is a sign that your body still isn't processing glucose well and you may need to address some of the common drivers.
Drivers of Insulin Resistance...
Poor Diet 🍰
High levels of pro-inflammatory omega 6 fats from industrial seed oils or factory farmed meat, low intake of fibre and a high consumption of alcohol, refined sugar and trans fat, can all drive insulin resistance.
Meal frequency may be important, as constant snacking or grazing throughout the day can keep blood glucose and insulin levels elevated.
It is important for women with PCOS to find their unique carb tolerance, in order to prevent insulin spiking too high or the stress of not eating enough. Your energy levels, sleep quality, mood and cravings can help you to figure out what works best for you.

Nutrient Deficiencies ⬇️
Poor soil quality, medication use, restrictive diets and chronic stress can all lead to nutrient deficiencies. The most important nutrients for insulin sensitivity and blood glucose control are magnesium, chromium, potassium, zinc, taurine, manganese and inositol. Most of these work by improving the metabolism of glucose and the insulin receptor sites.
Your body will always prefer nutrients from FOOD, rather than supplements, because in nature, foods contain a combination of synergistic nutrients which all work together. If we rely on supplements for our nutrient intake, this can lead to imbalances and skewed ratios. That being said, high quality, practitioner grade supplements can be helpful.
Lack of Sleep 😴
If you are skimping on sleep, or the quality isn't great, this will worsen your insulin sensitivity the next day, making your body less able to process glucose (carbs) efficiently. A lack of sleep can also throw off your energy levels, mood, appetite and cravings the next day. You will probably be more like to skip the gym and instead grab a takeaway on the way home from work.
When we sleep, our body is able to physically repair, especially between the hours of 10pm and 2am. If we work the night shift or regularly stay up late to binge watch Netflix, then our body is more likely to be in a state of chronic inflammation, which is a precursor of insulin resistance.
High Cortisol 🤯
Ahhh stress. There is just no escaping it, living in this modern world. When we are stressed (because of a real or perceived threat), this triggers our adrenal glands to pump out hormones like cortisol and adrenaline. One of their main roles is to release glucose from storage sites (like the liver), into the bloodstream to use as fuel. If this happens too frequently or for too long, blood glucose levels (and therefore insulin) can become elevated.
High cortisol levels also promote inflammation and deplete nutrients like magnesium, which can impair the function of the insulin receptors

Gut Dysbiosis 🦠
If you have an overgrowth of pathogenic bacteria, intestinal permeability (aka 'leaky gut'), and yeast or parasitic infections, this could impact your digestion and absorption of the nutrients needed for healthy blood glucose regulation.
As 70-80% of your entire immune system is located in your gut, any imbalances in this location can lead to chronic inflammation and stress throughout the body. Women with PCOS tend to have higher levels of 'bad bacteria' and low diversity within the gut.
The outer membrane of certain bacteria contains a toxin known as lipopolysaccharide (LPS). When levels are high, this is known as metabolic endotoxemia, which has been shown in studies to promote inflammation, weight gain and therefore insulin resistance.
Chronic Inflammation 🔥
It has been known for decades that the pro-inflammatory cytokine TNF-α was able to induce insulin resistance because of it's local (and potentially systemic) effects on metabolism, and that high doses of anti-inflammatory compounds are able to reverse this.
These pro-inflammatory cytokines can be produced as a result of a poor omega 3 to omega 6 ratio, food sensitivities, insufficient sleep and chronic over exercise. Inflammation is beneficial to a point, however it is when it becomes chronic and uncontrolled that it can start to damage tissues and potentially lead to health issues.
Inflammation is one of the 'root causes' of PCOS partly because of its impact on insulin sensitivity, but also due to its ability to up-regulate the 5-alpha reductase enzyme. This enzyme metabolises androgens into dihydrotestosterone (DHT) which is an androgen that is 3x more potent than testosterone.
Low Thyroid Function 🦋
The main thyroid hormones T4 and T3 are involved in glucose metabolism and insulin sensitivity. The thyroid is our master metabolism gland and almost every single cell in our body has a receptor site for thyroid hormone.
Low thyroid function can be caused by factors such as autoimmunity, nutrient deficiencies and chronic stress. Low T3 in particular, which is the 'active' thyroid hormone, has been associated with increased inflammation.
It is believed that 25% of women with PCOS actually have a thyroid issue, which could actually be driving the irregular ovulation and insulin resistance issues. Poor thyroid function, along with insulin resistance, inflammation and stress are some of the biggest drivers of PCOS.
Body fat levels 🔎
Insulin resistance can lead to weight gain and obesity, and a high body fat level can exacerbate insulin resistance. It works both ways. Fat cells are actually mini endocrine organs that can produce hormones like oestrogen and release inflammatory cytokines.
When oestrogen is elevated, this increases a hormone known as thyroid binding globulin (TBG) which can lower circulating thyroid hormones. As I have already discussed, low T4 or T3 can have a negative impact on insulin sensitivity.
If oestrogen levels are too low (due to a low fat diet, ageing or low body fat levels), this can also impair our insulin sensitivity, as oestrogen, (when at optimal levels) helps to improve insulin sensitivity. This is why we tend to be more insulin sensitive and able to tolerate more carbohydrates during the first half of our menstrual cycle (follicular phase), as we are naturally 'oestrogen dominant' at this time.
Environmental Toxin Exposure ☢️
Women with PCOS are like 'canaries in the coal mine', when it comes to environmental toxins. I believe that we tend to display the harmful effects of these chemicals before others do. There is actually quite a lot of evidence to show that exposure to endocrine disrupting chemicals like bisphenol A (BPA) in utero, can actually alter genetic expression and predispose women to develop PCOS later in life.
An increasing amount of evidence has linked exposure to toxins with both obesity and diabetes because of their ability to cause inflammation, immune dysregulation, mitochondrial dysfunction and impair thyroid health. Compounds such as BPA (found in plastic), have been labelled as 'obesogens', for this reason.
Sedentary Lifestyle 🛌
As humans, our genes expect us to move and be active every single day. Because of the conveniences of cars, public transport, online delivery and supermarkets, we are becoming more and more sedentary, which has a massive impact on our insulin sensitivity.
Women with PCOS benefit from daily movement and particularly strength training, as muscle helps us to uptake glucose from the bloodstream, without the need from insulin. One study found that physical inactivity was associated with the development of insulin resistance, dyslipidemia (abnormal lipid levels), increased blood pressure, and impaired microvascular function in healthy volunteers.
How to test…
The best ways to test for insulin resistance are to request the following blood tests from your GP:
HBA1C, fasting blood glucose, fasting insulin levels and a 2 hour oral glucose tolerance test (OGGT).
(Lab measurements and units differ depending what country you are in)
You can also monitor your blood glucose levels at home using a glucometer to see how much your levels increase 1 and 2 hours after eating. Most of us respond differently to different types and amount of carbohydrates, so you may need to experiment to find which work best for you.
It is important to note that all of your labs may come back 'normal', however you could still be dealing with insulin resistance, so don't rule it out. In some cases insulin is so high that blood glucose levels don't elevate much at all, and the glucose is immediately stored as glycogen and fat tissue.
What you can do...
1. Optimise Your Diet 🍎
Ditch the processed foods and JUST EAT REAL FOOD #JERF. Increase your intake of anti-inflammatory fats & proteins like eggs, organic dairy (if tolerated), wild fish and high quality animal products like grass fed beef, as these are the building blocks to your hormones like progesterone.
When consuming healthy carbs like sweet potatoes, squash, fruit, oats and quinoa, make sure that you consume them alongside a source of protein and healthy fat, to reduce the blood sugar spikes. Your body can also process carbs better during the post-workout window, so you may benefit from consuming more of your carbs around workouts!
Aim for 3 balanced meals per day (& 1-2 snacks if needed), with around 3-4 hours between each, as this allows glucose & insulin levels to fall before eating again, whilst supporting your adrenals & thyroid.
2. Restore Nutrient Deficiencies ⬆️
Eat a nutrient dense diet including foods such as organ meats, pasture raised eggs, grass fed beef, organic berries and cooked leafy green vegetables. Avoid consuming a lot of foods that contain anti-nutrients, such as grains, soy, nuts, seeds, beans and legumes, or at least make sure you prepare them properly to reduce the levels of natural compounds like phytates and lectins.
Consider supplementing with specific insulin sensitising nutrients based on your needs. I recommend working with a skilled practitioner who can help you with this. If you are already eating a great diet, make sure that you are digesting and absorbing these too! Low digestive enzyme production and/or stomach acid (HCL) may prevent this.
3. Get Enough Sleep 💤
Aim to be in bed for 10.30pm at the very latest, so that you can benefit from at least some of the regenerative and healing that takes place between 10pm-2am. If you are waking up super early to hit the gym, you may actually benefit from some extra time in bed!
Respect the light and dark cycles of nature, by getting out in the sunlight during the day and then avoiding blue light exposure from technology past 8pm. I also recommend using tools like F.LUX on your laptop or 'night shift' on your smart phone to filter the blue light levels after sunset.
Work on your sleep hygiene and evening routine if you struggle with disturbed sleep, difficulty falling asleep or fatigue upon waking. This could involve taking an epsom salt bath, keeping your bedroom cool, purchasing black out curtains & diffusing essential oils.
4. Manage stress 🧘🏻♀️
Stress is inevitable, but it how we manage and respond to it that is important. The negative thoughts you think can trigger a stress response similar to if you were being chased by a lion. Use tools like journalling, therapy, yoga or meditation to help you to manage your mindset and stop being so reactive. Take time every day to put your body in the parasympathetic (rest and digest) nervous system state. This will be different for everybody, so it is important to find what works for you. This could be dancing, colouring, singing, reading a book, playing with your dog or going for a walk in nature.
Having PCOS in itself is pretty stressful, because of the frustrating symptoms that it can cause, (acne, face and body hair growth, hair loss on your head, weight gain to name a few!) In fact, women with PCOS tend to have higher levels of cortisol than women without.
Investing in support from a skilled practitioner whilst on your healing journey, can be a great way to reduce the stress and pressure of having to figure this all out on your own. When my hormonal issues were at their worst, hiring a coach helped me SO MUCH!
5. Fix Your Gut 💩
Even if you aren't displaying obvious signs of poor gut health such as bloating, constipation, diarrhoea or reflux, it is still possible to have dysbiosis, infections and 'leaky gut'. If you have addressed all of the other factors in this list and are still struggling with insulin resistance and PCOS symptoms, I would highly recommend investigating your gut.
You may benefit from a full gut healing protocol which involves eradicating any infections present, replacing the digestive enzymes that may be lacking then 'healing and sealing' the gut lining with a range of specific nutrients.
6. Reduce inflammation 🔥
Start by eating an anti-inflammatory diet which cuts out processed, packaged foods and particularly omega 6 rich fats. We need some omega 6's to help regulate inflammation, but ideally we should aim to keep them in a 3:1 ratio with omega 3's. Fats and oils to limit/avoid include industrial seed oils (sunflower, canola, rapeseed, soybean etc), conventionally raised meat/dairy products and large amounts of nuts and seeds.
Making your own meals from scratch at home using good quality organic produce would already help a ton as many restaurants & food establishments use industrial seed oils.
7. Improve Thyroid Function 🦋
In order to rule out poor thyroid function, you will need to run a FULL thyroid panel including TSH, T4, T3, reverse T3 and antibodies. Most conventional doctors and endocrinologists will only run TSH and T4 at the most, which isn't enough. Your TSH and T4 may be completely 'within range', however you could have low T3 (active hormone) and/or elevated antibodies, which indicates Hashimotos Thyroiditis.
A thyroid condition almost never occurs alone. In my clinical experience, there is always an adrenal issue coinciding, and may actually be the underlying cause of hypothyroidism. Your adrenals, thyroid and ovaries are best friends and when one of these glands are out of whack, the others will be thrown off shortly after. For this reason, stress management is crucial, when trying to overcome a thyroid issue.
8. Maintain a Healthy Weight ⚖️
The goal is to be at a healthy body weight for our height and current needs. If you are currently OVER weight, avoid crash diets and instead focus on nourishing your body with real, whole foods. It may be helpful to track your caloric intake for a few days using an app like My Fitness Pal, as it is possible to be over consuming even 'healthy foods' like nuts, avocado and coconut oil. Most women need around 2,000 calories per day, however you may need more or less depending on your activity levels and health status etc.
If you are UNDER weight, make sure you are eating (and digesting) enough healthy fat like coconut products, eggs, grass fed butter/ghee, olive oil etc, to provide your body with the building block to your hormones, which is cholesterol. Avoid intense activity like HIIT or chronic cardio, as these can stress your body out and lead to depletion.
9. Clean up your Environment 🌿
We cannot totally avoid exposure to chemicals such as BPA, phthalate and heavy metals, however we can make changes to our home environment to reduce our levels. Avoid plastic by storing food in glass Tupperware and buying a stainless steel reusable water bottle. Swap your conventional personal care products for non-toxic, organic brands. Filter the tap water in your home. Buy organic food as much as frequently as possible.
You can also support your liver and detoxification pathways through sweating, exercise, sauna, dry body brushing, coffee enemas and herbal medicine, to support your body in eliminating these compounds. It is essential that you are having at least one bowel movement every day, otherwise these toxins can be recirculated.
10. Lift weights & walk 💪🏼
As I have discussed, the more lean muscle mass we have, the more effectively we can metabolise glucose. Lift some heavy weights ladies and don't worry, you won't get bulky! Pay extra attention to your legs and glutes as these are the largest muscles in your body.
That being said, more exercise (or intensity) isn't better. Over training (or under recovery), can be just as detrimental for women with PCOS, as it can raise cortisol and inflammation levels. Stick with 3-5 workouts per week, with a mix of strength training, longer walks and restorative exercise like yoga or pilates.
Aim for 10,000 steps daily as a way to increase your non-exercise activity thermogenesis (NEAT). To further support your body in utilising blood glucose after eating, go for a 10-20 minute brisk walk after each meal.
Want my COMPLETE ROADMAP to overcoming YOUR PCOS symptoms? Check out my self-paced online course PCOS SUCCESS.
In this course I share everything that I know about healing the underlying causes of PCOS naturally.
Get lifetime access, hours of educational content & recommendations from an experienced practitioner NOW & stop trying to figure it all out on your own.
>> CHECK OUT PCOS SUCCESS <<
Don't miss a beat!
New moves, motivation, and classes delivered to your inbox.
We hate SPAM. We will never sell your information, for any reason.

